Migraines are a peculiarly painful condition. They affect millions of people worldwide, and can strike without warning or relief for hours or days on end. In fact, migraine is now ranked as the second leading cause of years lived with disability, following only lower back pain. Scientists still don’t understand exactly why migraines happen, nor how to cure the condition – but perhaps cannabis can help.
Cannabis users have been reporting anecdotal relief for years, but it’s only recently that research has begun to dig into the complexities of migraines and how – or why – cannabis may be able to bring relief.
Based on the limited existing evidence, the best cannabis strain for migraines may be a Type II that includes both THC and CBD, and a terpene profile that includes beta-caryophyllene, myrcene, linalool, limonene, bisabolol, humulene or pinene. Treating migraine pain is one of the instances where inhaled cannabis consumption, such as smoking or vaping, is important for the right effects and speed of delivery. Edibles won’t produce the same experience, but topicals may be able to help, too.
In searching for the best strain for migraine relief, it’s important to remember that strain names are an unreliable indicator of experience. This article includes strain names as a starting point for you to find flower or products near you that match the chemical makeup, not the exact strain name.
Strain names mentioned in this article include:
The difference between migraines and headaches
A headache is a vague term that can apply to many different types of head pain, so it’s important to get specific.
There are over 150 types of headaches, all of which fall under the categories of primary or secondary headaches. A primary headache, such as a migraine, is its own condition, and not caused by a separate condition. A secondary headache is a symptom of another medical issue.
Other common types of headaches include tension headaches, cluster headaches, and sinus headaches. Cluster headaches can be mistaken for migraines because they’re painful, but they tend to happen in clusters of frequent, severe, and sudden headaches that often occur at the same time each day or the same seasonal change.
The science of migraines
Migraines are not just “bad headaches.” Migraines are a neurological disease that causes recurring episodes of throbbing, pulsing, or stabbing pain on one or both sides of the head, as well as the eyes, temples, jaws, sinus, or neck. Symptoms also include nausea, numbness, tingling, visual disturbances, sweating or chills, and/or light and sound sensitivity. Migraines affect the blood flow in the brain as well as levels of other important chemicals. For example, researchers at Hopkins Medicine point to changes in chemical compounds like CGRP, serotonin and hormones like estrogen affecting pain levels.
The Cleveland Clinic estimates around 12% of Americans suffer from migraine disorders, and is the 6th most disabling disease worldwide.
Scientists still don’t fully understand migraines, although a lot of knowledge regarding the cause of migraines has been gained in recent years. The condition is thought to be genetic, and known to be triggered by stress as well as a range of other factors, like hormones and weather changes. It occurs more frequently in women than men (women are three times more likely to get migraines), but what triggers an episode, what can stop an episode, and the frequency of episodes are still being researched.
There are also multiple types of migraines. These include:
- Migraine with aura – an aura is a symptom that precedes a migraine, such as blind spots, bright flashes, numbness, tingling, or speech disturbances. An estimated 20% of people who have migraines get auras before they start.
- Migraine without aura – a migraine that strikes without warning
- Migraine aura without headache – a migraine that includes an aura; often includes visual or sensation symptoms, but no head pain
- Migraine with motor aura (previously hemiplegic migraine) – includes temporary paralysis on one side of the body
- Retinal migraine – includes a partial or total loss of vision during the migraine, but in only one eye.
- Chronic migraines – severe headaches that happen at least 15 days per month
- Migraine with brainstem aura (previously basilar migraine) – symptoms of the aura include vertigo, slurred speech, double vision, loss of balance, ringing in ears, and nausea.
- Status migrainosus – migraine attacks that last longer than 72 hours.
What makes migraines so frustrating to deal with is that episodes go beyond just head pain. Migraines can happen suddenly and without warning but last hours. Some people have identifiable symptoms that precede an episode while others are left to the whims of the disease. Migraines are also highly specific to each person – what helps or works for one person may not touch another’s pain. Finding the right relief for your migraine pain is a lot like finding the cannabis routine that works for you – it takes time, tracking, and trial and error.
Migraine episodes go through a series of phases, each with its own pain and symptoms. These phases are
- Prodrome – can precede the headache by hours or days. Symptoms include tiredness, irritability, moodiness, and cravings. An estimated 75% of people with migraines go through the prodrome phase, even if they don’t recognize it.
- Aura – precedes the headache by 1 – 2 hours and includes visual, sensory, or speech disturbances, but only affects around 20% of migraine sufferers.
- Headache – the most painful phase of the migraine cycle, which can last between four and 72 hours
- Postdrome – the “migraine hangover” which can last up to 48 hours
Migraine pain is debilitating. When every light or noise is like a jackhammer on the side of your head, you can’t move without making the pain or nausea worse, and even water won’t stay in your stomach, it can be impossible to go about your day. Migraines can cause people to suddenly call off work, cancel plans, and lose out on opportunities in order to deal with their pain. Chronic migraines can make it incredibly challenging to hold down a job. The fact that migraine is now ranked as the second leading cause of years lived with disability illustrates the magnitude of the negative impact of the disease to patients and their ability to function normally.
And the suffering doesn’t end when the headache does. Many people who suffer from migraines also go through a “postdrome” phase, best described as a migraine hangover that can last for up to two days. The Cleveland Clinic estimates 80% of people who get migraines also go through postdrome, prolonging the suffering.
Many people who suffer from migraines may reach for over-the-counter medications to reduce pain and be able to continue with their day. But this comes with another potential problem, as relying too heavily on certain medications can cause rebound headaches (also known as medication overuse headache).
How cannabis can help with migraines
So how can cannabis help? Like many conditions that modern medicine falls short of treating, migraines are now suspected to be a possible problem of endocannabinoid system deficiency in some patients. The endocannabinoid system is a complex neurologic system with receptors on every organ in your body. The ECS appears in every mammal on the plant, as well as a few other species.
Although it wasn’t identified until the 1990s, scientists today believe this system to be of massive importance in overall health. The ECS touches on nearly every biological function you have, including sleep, pain, appetite, body temperature, immune function, memory, and hormone regulation. The two most studied receptors in the system are the CB1 and CB2 receptors.
Home remedies for dealing with migraines often involve changing the setting you’re in to a quiet, dark room as well as breathwork and meditative practices. Since these practices are known to stimulate the endocannabinoid system, they can be additionally beneficial.
The endocannabinoid system and migraines
Studies around migraines and cannabis are limited but expanding. While migraines are a commonly reported condition by patients in cannabis studies, there is little clinical research on how cannabis can influence migraine pain.
- A review of existing endocannabinoid system and migraine research from March 2022 identified many surveys, but fewer clinical research trials, and even fewer double-blind placebo studies. The authors noted that while “promising data are emerging on the possible role of ECS in migraine…proper placebo-controlled trials are needed to establish a therapeutic role for cannabinoids.” 1
- A 2008 study found serotonin and endocannabinoid levels, including anandamide, were lower in people with chronic migraines. 2
Endocannabinoids have been linked to an area of the brain called the trigeminovascular system, thought to play an important role in all headaches, including migraines. This system shows up in several studies.
- In a 2016 paper, Dr. Ethan Russo concluded a “possible relationship of migraine with the ECS is highlighted by numerous findings” and “great deal of additional support for the integral role of the ECS in migraine pathophysiology has been provided by a series of investigations linking endocannabinoids to the trigeminovascular system.” He also noted “repetitive administration with a TRPV1 agonist such as CBD27 could conceivably desensitize the receptor and thus alleviate these pathophysiological mechanisms.” 3
- A 2009 study touched on the trigeminal system as well, examining the connection between the CB1 gene (called CNR1) and people who reported migraines. Scientists found a “significant…effect of CNR on migraines”, suggesting a “significant effect of CNR1 on migraine headaches that might be related to the alteration of peripheral trigeminovascular activation.” 4
- A 2004 study found that the endocannabinoid anandamide can inhibit trigeminal neurons, which suggests a way in which endocannabinoids may be able to prevent migraines. 5
THC and migraines
THC is well-known for its anti-nausea and pain-relieving effects. Since pain and nausea are two of the most common symptoms of migraines, this cannabinoid is of great scientific interest in helping people who suffer from migraines.
- A 2019 retrospective review of 316 patients found that medical cannabis improved the experience of 88.3% of people while decreasing the frequency of episodes by an average of 42% (although some people saw a 50% decrease or more). Researchers also noted that a 20:1 THC to CBD ratio was more beneficial than a 1:1. 6
- A 2018 study of a medical cannabis cohort made note of the fact that THC enhances analgesia (pain relief) and is 20 times more anti-inflammatory than aspirin. The study called out pinene, myrcene, and beta-caryophyllene as specifically useful terpenes. Higher THC strains were also more commonly used for migraine. Researchers also noted that “vaporizing or joint use were the primary methods of use across all groups.” 7
- A 2021 study of a medical cannabis cohort reported that high THC / low CBD flower was the most preferred cannabis type in migraine patients. Of 346 migraine patients, 3 in 4 preferred cultivars were high THC / low CBD, with “Headband” (22-24% THC, < 1% CBD), “Warlock CBD” (8-11% THC, 8-11% CBD), and “Master Kush” (24-26% THC, < 1% CBD) all tied for the top choice. All 3 had β-caryophyllene as 1 of the top 3 terpenes, along with a mix of linalool, limonene, β-myrcene, bisabolol, and humulene. 8
- A 2018 animal study using THC on rats concluded that “THC reduces migraine-like pain when administered at the right dose” and there is “anecdotal evidence for the use of cannabinoids as a treatment for migraine in humans and implicate the CB1 receptor as a therapeutic target for migraine.” 9
- A 2016 retrospective study of 121 adults with migraines out of Colorado found that using cannabis reduced the average frequency of migraines from 10.4 to 4.6 headaches per month. Daily cannabis consumption was an effective treatment for 85% of participants. Researchers noted inhaled cannabis was most common and effective, while edibles had a higher rate of negative effects. 10
- A 2001 review paper by cannabis researcher Dr. Ethan Russo details the historical use of cannabis for migraines. Russo concluded the evidence he examined “supports experimental protocols of cannabis usage in migraine treatment should go forward employing modern controlled clinical trials.” 11
CBD and migraines
Although CBD is sometimes considered the “more medicinal cannabinoid” because it’s not intoxicating, there is less research on its effects on migraines.
- A 2021 review of research on cannabis and migraines concluded that CBD could be effective, but more consistent dosing is needed than with THC alone. Researchers suggest taking CBD three times a day, starting with a low dose and increasing it as needed. 12
- The same 2018 study of a medical cannabis cohort noted that CBD is several hundred times more anti-inflammatory than aspirin and some patients with headaches preferred higher CBD strains (while most preferred higher THC strains).
How to choose the best cannabis strain for migraines
To find the best strain for providing migraine relief, skip over the indica/sativa classification. These misused terms simply differentiate between cannabis indica and cannabis sativa plants but tell you almost nothing about the chemical composition of the nugs, which is what you really need to know.
Don’t get too hung up on strain names either. While these are fun marketing terms, there are no standardized regulations or qualifications for what constitutes a specific strain. As such, growers in different states, or even within the same state, can sell products with wildly different chemical compositions (providing different experiences) under the same strain name.
The first piece of information you genuinely need is the chemotype of your cannabis. Chemovars classify cannabis based on the dominant cannabinoid, and there are three main types on the market right now.
- Type I: high THC, low CBD
- Type II: balance of THC and CBD
- Type III: low THC, high CBD
The best strain for treating migraines may be a Type II cultivar, because a balance of THC and CBD may be needed to mitigate the symptoms of a migraine. As the 2016 Colorado study pointed out, the success of THC in treating a migraine is dose-dependent, and it’s easy to have too much. THC has bi-phasic effects, so what helps at a low dose could hurt at a high dose. A typical recommended daily dose of THC is between 15 – 30 mg, and it’s easy to exceed that with a bowl pack or a joint roll of 18% or 25% cannabis.
Both CBD and THC can interact with other medications, so always talk to your medical professional before starting cannabis products to ensure your safety.
The best way to consume cannabis for migraines
The best way to consume cannabis to help your migraine is personal, but inhaled applications seem to provide the best results for abortive effects – the fast onset for “as needed” relief at the beginning of a migraine attack. Inhaled cannabis such as smoking or vaping, delivers nearly immediate effects, and that efficacy of delivery can be important for people who are trying to work around migraines and abort it quickly. In addition to the analgesic effects, THC also has anti-nausea effects that are helpful for some with migraines.
Topical cannabis products can also be useful, but research and data is very limited. These products deliver the cannabinoids to receptors in your skin or cross through the skin barrier into the bloodstream, with transdermal products. For migraines, cannabis topicals are typically applied directly to the neck and shoulders area to help combat tension and inflammation, and can also be applied directed to the temples as an attempt to get cannabinoids as close to the sources of the headache as possible. Cannabis topicals can be a good option for people who don’t want to get high or need migraine relief in a situation where being high is not an option, such as in the workplace.
Edibles are another option, but as noted in several of the studies mentioned, edibles had the most negative side effects of any delivery method. Since nausea is a common side effect of migraines, eating a sugar-filled gummy may not be the best option. Moreover, edibles take significantly longer to take effect, so they are not good options for abortive (as needed) migraine use. However, they may have a role in chronic pain conditions when used as a maintenance treatment, with vaporizing added on for abortive use during migraine attacks.
Best terpenes for migraines
Cannabinoids aren’t the only important chemical compound in picking out strains for migraines – the terpene profile is also important. While there is limited research on cannabis terpenes specifically, there is ample research on essential oils and aromatherapy for migraines. The key point is that the cannabinoids and terpenes work synergistically together (cannabis entourage effects), better than each individual component alone.
Beta-caryophyllene
- A 2021 paper from the American Headache Society examined the most popular strains consumed by people with migraines and found the top three strains were dominant in beta-caryophyllene. The study also noted 64% of patients preferred to inhale their cannabis.
- In Dr. Ethan Russo’s 2001 review on cannabis and migraines, he specifically named beta-caryophyllene as one of the top terpenes for migraine relief.
Myrcene
- The 2018 study of a medical cannabis cohort noted that along with beta-caryophyllene, myrcene was the most popular terpene in popular strains named by patients.
Pinene
- A 2021 review of terpene-based medicines for brain health pointed to several studies that showed pinene reduced pain associated with migraines and there was “evidence [to] suggests pinene… provides analgesia in migraine-associated pain.” The authors point to pinene’s anti-inflammatory properties as the main reason for these effects. 13
- Rosemary oil, which is high in pinene, is a common tool of aromatherapy for its anti-inflammatory properties and is known for reducing pain. 14 15
- Pinene was the other terpene specifically mentioned for pain relief by Russo in his 2001 review on migraines and cannabis.
Linalool
- A 2012 clinical trial with 47 patients tested the effects of inhaled lavender oil (main terpene linalool) on migraine head pain. Over 70% of cases responded “entirely or partially” to the lavender oil, suggesting inhaled linalool may help treat migraine pain. 16
- The 2021 review of terpene-based medications that mentioned pinene also identified linalool as a key candidate for further research for an array of brain conditions that included migraines.
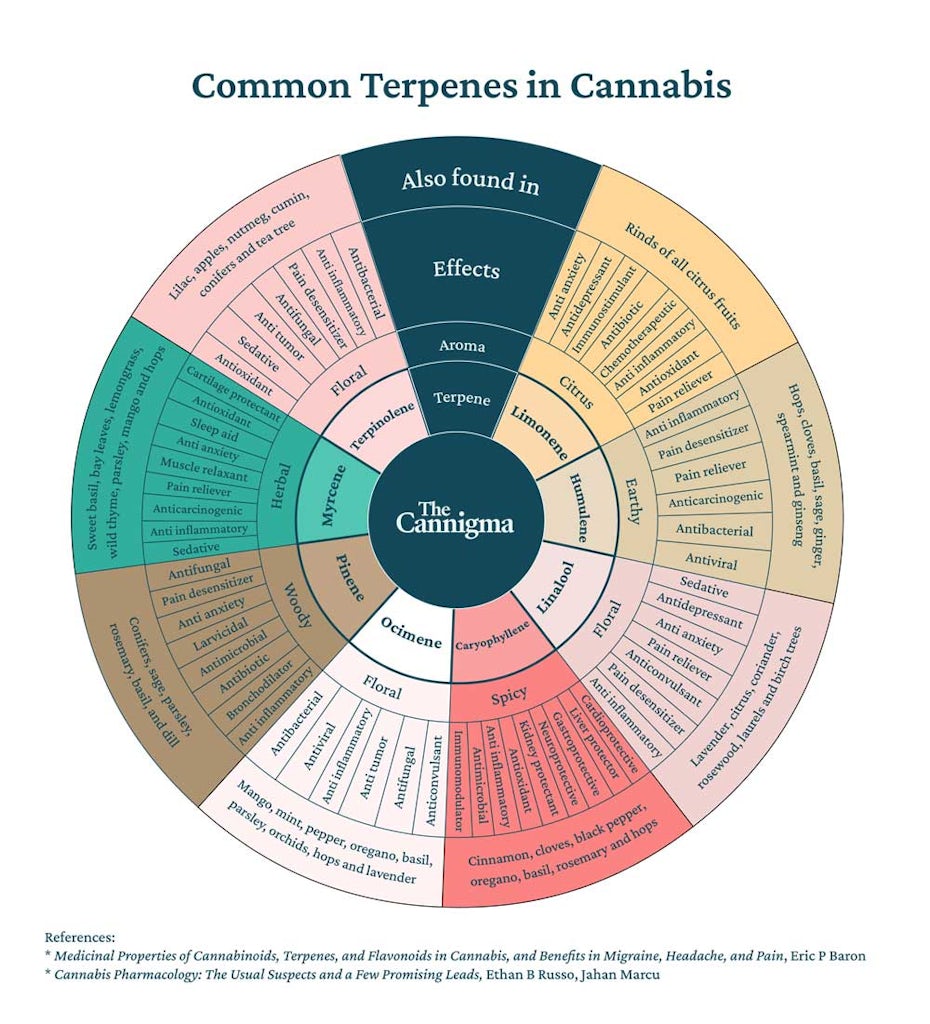
If you don’t have access to lab reports that tell you the terpene profile of your weed, or you can’t identify terpenes by smell, you can always use essential oils to complement your cannabis routine and dial in the effects you’re looking for.
The best strains for migraine pain
The best strains to treat migraine pain may be a Type II with a balance of CBD and THC and includes a terpene profile of beta-caryophyllene, pinene, linalool, limonene, bisabolol, humulene, or myrcene. Strains with this profile include Critical Mass and Cannatonic.
Type II strains are extremely hard to come by in today’s cannabis market. If you aren’t able to find a strain with a balance of cannabinoids, you can always supplement by blending CBD flower into your THC flower or taking a CBD tincture prior to consuming THC. Type I strains that fit this terpene profile include Forbidden Fruit, Blue Dream, and AK-47. However, Type I cultivars will also have a much higher side effect profile including psychoactive effects, which limit where and how much it can be used.
The most popular strain named in several of the aforementioned studies is also a Type I, called OG Shark, which has a THC content of 20% or more and comparatively little CBD. The terpene profile includes caryophyllene, myrcene, and linalool, among others.
You don’t need to find these exact strains, but rather use their chemical composition as a starting point to finding strains available to you that match these criteria. Ask to see a certificate of analysis when possible to get detailed information on the chemical composition of your weed. If that’s not possible, ask to smell the weed before you buy it to try to identify the terpene profile.
The bottom line is that there is a limited but growing body of evidence on the use of cannabis and migraine treatment in terms of specific recommendations. A lot more research is needed to further define optimal strains, cannabinoid, and terpene ratios for migraine treatment.
With that said, it is unlikely there will be one single strain useful for all patients with migraine. Just like medications, it can be a trial and error process to see what you respond to best. Some patients respond very well to some migraine medication classes and types, whereas others do not at all. Some patients have a lot of side effects to some medications, whereas others do not at all to the same medicine. Cannabis is likely similar in that there may be common chemovar strains that in general are often helpful to many people. However, finding the specific chemovar or strain for you that you also tolerate well may take several different trials in fine-tuning which works best for you.
Sources
- Lo Castro F, Baraldi C, Pellesi L, Guerzoni S. Clinical Evidence of Cannabinoids in Migraine: A Narrative Review. J Clin Med. 2022 Mar 8;11(6):1479. doi: 10.3390/jcm11061479. PMID: 35329806; PMCID: PMC8949974.
- Rossi C, Pini LA, Cupini ML, Calabresi P, Sarchielli P. Endocannabinoids in platelets of chronic migraine patients and medication-overuse headache patients: relation with serotonin levels. Eur J Clin Pharmacol. 2008 Jan;64(1):1-8. doi: 10.1007/s00228-007-0391-4. Epub 2007 Nov 15. PMID: 18004553.
- Ethan B. Russo. Clinical Endocannabinoid Deficiency Reconsidered: Current Research Supports the Theory in Migraine, Fibromyalgia, Irritable Bowel, and Other Treatment-Resistant Syndromes. Cannabis and Cannabinoid Research.Dec 2016.154-165.https://doi.org/10.1089/can.2016.0009
- Juhasz G, Lazary J, Chase D, Pegg E, Downey D, Toth ZG, Stones K, Platt H, Mekli K, Payton A, Anderson IM, Deakin JF, Bagdy G. Variations in the cannabinoid receptor 1 gene predispose to migraine. Neurosci Lett. 2009 Sep 18;461(2):116-20. doi: 10.1016/j.neulet.2009.06.021. Epub 2009 Jun 17. PMID: 19539700.
- Akerman, S., Kaube, H., & Goadsby, P. J. (2004). Anandamide is able to inhibit trigeminal neurons using an in vivo model of trigeminovascular-mediated nociception. The Journal of pharmacology and experimental therapeutics, 309(1), 56–63. https://doi.org/10.1124/jpet.103.059808
- Medical Cannabis for Chronic Migraine: A Retrospective Review (P3.10-015) Laszlo Mechtler, Vincent Bargnes, Paul Hart, Jennifer McVige, Nicolas Saikali. Neurology Apr 2019, 92 (15 Supplement) P3.10-015;
- Baron, E. P., Lucas, P., Eades, J., & Hogue, O. (2018). Patterns of medicinal cannabis use, strain analysis, and substitution effect among patients with migraine, headache, arthritis, and chronic pain in a medicinal cannabis cohort. The journal of headache and pain, 19(1), 37. https://doi.org/10.1186/s10194-018-0862-2
- Ibid
- Kandasamy R, Dawson CT, Craft RM, Morgan MM. Anti-migraine effect of ∆9-tetrahydrocannabinol in the female rat. Eur J Pharmacol. 2018 Jan 5;818:271-277. doi: 10.1016/j.ejphar.2017.10.054. Epub 2017 Oct 28. PMID: 29111112; PMCID: PMC5742305.
- Rhyne DN, Anderson SL, Gedde M, Borgelt LM. Effects of Medical Marijuana on Migraine Headache Frequency in an Adult Population. Pharmacotherapy. 2016 May;36(5):505-10. doi: 10.1002/phar.1673. Epub 2016 Jan 9. PMID: 26749285.
- Russo, Ethan. (2001). Hemp for Headache: An In-Depth Historical and Scientific Review of Cannabis in Migraine Treatment. Journal of Cannabis Therapeutics. 1. 10.1300/J175v01n02_04.
- Mechtler, L.L., Gengo, F.M. & Bargnes, V.H. Cannabis and Migraine: It’s Complicated. Curr Pain Headache Rep 25, 16 (2021). https://doi.org/10.1007/s11916-020-00931-2
- Weston-Green K, Clunas H, Jimenez Naranjo C. A Review of the Potential Use of Pinene and Linalool as Terpene-Based Medicines for Brain Health: Discovering Novel Therapeutics in the Flavours and Fragrances of Cannabis. Front Psychiatry. 2021 Aug 26;12:583211. doi: 10.3389/fpsyt.2021.583211. PMID: 34512404; PMCID: PMC8426550.
- Babar Ali, Naser Ali Al-Wabel, Saiba Shams, Aftab Ahamad, Shah Alam Khan, Firoz Anwar. Essential oils used in aromatherapy: A systemic review, Asian Pacific Journal of Tropical Biomedicine, Volume 5, Issue 8, 2015, https://doi.org/10.1016/j.apjtb.2015.05.007.
- Raskovic, A., Milanovic, I., Pavlovic, N., Milijasevic, B., Ubavic, M., & Mikov, M. (2015). Analgesic effects of rosemary essential oil and its interactions with codeine and paracetamol in mice. European review for medical and pharmacological sciences, 19(1), 165–172.
- Sasannejad P, Saeedi M, Shoeibi A, Gorji A, Abbasi M, Foroughipour M. Lavender essential oil in the treatment of migraine headache: a placebo-controlled clinical trial. Eur Neurol. 2012;67(5):288-91. doi: 10.1159/000335249. Epub 2012 Apr 17. PMID: 22517298.
Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support